COVID-19 Anxiety and Stress
Advanced Therapeutic Solutions for Anxiety provides therapy for the treatment of COVID-19 anxiety and stress.
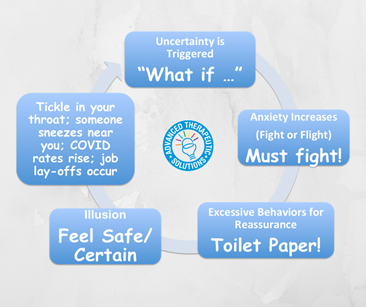
As reality of the COVID-19 pandemic sets in, so do the “what if” questions: What if I get COVID? What if this isn't clean? What if the kids get sick? Husband/Wife gets sick? What if my parents need help? What if they get sick, and I can’t go to them? What if the hospitals become too full? What if we don’t have enough food? What if the grocery store closes?
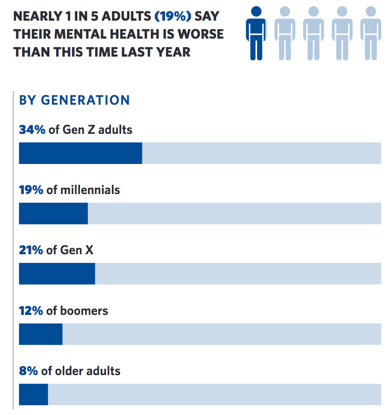
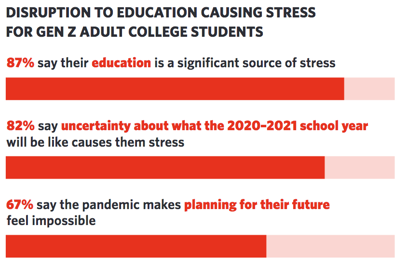
Even if you aren't feeling anxiety about contracting COVID-19, you may be feeling just as out of control about other aspects of your life that have been impacted by COVID-19. According to the American Psychological Association's Stress on America report that surveyed the mental health impact of COVID-19, Generation Z adults (ages 18-23) are reporting worse mental health problems than other generations, and Generation Z teens (ages 13-17) are reporting severely disrupted plans impacting their future. Their "What if" questions may be: What if I can't go back to school? What if I can't graduate on time? What if I can't plan my next steps? What if I can't get a job? Older generations (e.g., millennials, Generation X, Baby Boomers) may not have as much developmental disruption, but their "What if" questions may be about their security and that of their families: What if I lose my job? My business? My livelihood? How will I take care of my family?
We strive for control when things feel out of control. We try to continue our lives, but keep getting met with barriers. When we find a solution for one barrier, we hit another wall and have to find a solution for that barrier. It’s mentally, physically, and emotionally exhausting. We’re grieving our losses while fearing what is to come next.
The need for certainty is a key trigger for anxiety.
We can’t be 100% certain in life. So we try to do things that give us the illusion of certainty to calm those “What if” questions (excessively checking the news; worrying with every sniffle, cough, or sneeze; stocking up excessively on cleaning supplies, food, medicine; purchasing expensive sanitizing gadgets; checking your state’s COVID-19 tracker repeatedly; getting a blood test to check for antibodies; checking grades repeatedly; doing and redoing school assignments to perfection; avoiding work or school; checking to make sure you can taste and smell; checking your bank account repeatedly; looking for jobs - even though you have one - just in case you get laid off - even though your boss has reassured you, etc.). These behaviors may bring relief in the short-term, but then dissipate and the need to seek reassurance and certainty loops around again. The need for certainty triggers the fight or flight response, urging you to fight to protect yourself. Only there seems to be no rest, and also no certainty.
Learning how to tolerate uncertainty is a key feature of anxiety treatments.
We are living in the midst of a pandemic, where there is ambient anxiety all around us. If you are feeding the “What if” questions with behaviors meant to reassure you, then you are only feeding the anxiety, not the certainty. While COVID-19 is new to us, and research for an effective vaccine is pending, anxiety isn’t new, and treatments aren’t pending. We already know the evidence-based treatments that turn off the anxiety reinforcement loop. At ATSA, we use cognitive behavioral therapy and acceptance and commitment therapy to help you tolerate anxiety and continue to live a valued life in the midst of the current pandemic.
Read COVID-19 and Mental Health: A Growing Crisis by Mental Health America
Read Stress in America 2020: A Mental Health Crisis by the American Psychological Association
COVID-19 Anxiety Loop
Looking for the Child/Adolescent Page? Click here
Questions? View FAQs View Insurance InformationClinical Procedures for COVID-19 Anxiety and Stress Evaluation and Outpatient Treatment
Free Phone Intake Consultation
Up to 30-min phone consultation so we can hear about your presenting issue, the symptoms you are experiencing, when they started, the severity of symptoms, and if we are the appropriate place for your treatment. The diagnostic intake process is discussed, and your insurance/billing questions are answered. If the treatment you need is within our scope of services, we begin the scheduling process. If it is deemed that we are not the appropriate place, we will provide you with referrals and resources to help you. We want to make sure to connect you with services, and that includes helping you find treatment elsewhere if that's what you need.
Free
CPT CODE: 0
Diagnostic Evaluation
A 90-min diagnostic interview is conducted to assess the presenting problem, symptoms severity (onset, duration, frequency), review areas of life that have been impacted (daily functioning, work, home), collect history, including family history of anxiety or depression, and review what you hope to gain from treatment at ATSA. Specific questions and or measures may be administered during the session for diagnostic purposes.
Starting at 295
CPT CODE: 90791
Treatment Planning Session
A 60-min session to review how the first sessions have felt to you, present hypotheses, and collaborate on a treatment plan. Treatment approaches may include Acceptance and Commitment Therapy (ACT), Cognitive Behavioral Therapy (CBT), Exposure and Response Prevention (ERP). Treatment dose is also discussed, specifically if weekly 60-min outpatient sessions will be effective, or if intensive doses (e.g., 3-hr sessions) should be considered. Likewise, location of where sessions should occur for most effective outcome is also discussed and planned out. Decisions are made as to whether to start with therapy sessions only, allowing for the future addition of psychopharmacological treatment as an adjunct, or whether to start with combined treatment, (or in rare cases to start with psychopharmacological treatment before CBT, ACT, or ERP).
Starting at 175
CPT CODE: 90837
Exposure Clinic Session
60 min exposure sessions to present you with the phobic stimulus and begin the process of fear extinction. The key to exposure therapy is to activate new learning, which is done by presenting the phobic stimulus, and assisting you to approach (vs avoid) the stimulus, using a hierarchical approach. With repeated exposures, you gain distress tolerance and fear extinction. Additional therapies (e.g., ACT, CBT) may be applied to keep you focused and motivated in preparation for exposures, particularly when exposures become more challenging as we move up the hierarchy. When possible, family members will be included to learn how to facilitate approach coping and reduce enabling avoidance. Our data show that when family members learn how to support you, you are more likely to maintain your treatment gains.
Starting at 175
CPT CODE: 90837
Exposure Therapy in Home or Community Settings
60-min exposure sessions provided in the home or community setting to help transfer treatment gains into these domains. To increase transfer of treatment gains, reduce avoidance of the phobia across settings, and reduce others rescuing you from approaching your phobia (to rescue you from distress), in-vivo and in-situ exposure therapy is most effective. Not only will you develop distress tolerance, new learning, and fear extinction, so will others in these settings, which helps them reduce rescuing and enabling. Home visits are used to help you use skills at home, and Community sessions provide exposure practice in new settings.
Starting at 185 + travel
CPT CODE: 90837