COVID-19 Anxiety and Stress
Advanced Therapeutic Solutions for Anxiety provides therapy for the treatment of COVID-19 anxiety.
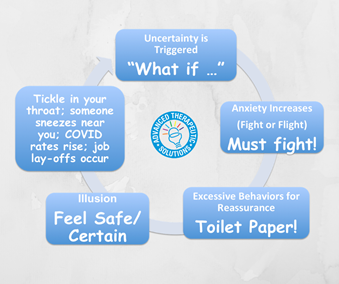
As reality of the COVID-19 pandemic sets in, so do the “what if” questions: What if I get sick? My mom gets sick? My dad? What if grandma/grandpa gets sick? What if we can’t go see them? What if the hospitals become too full? What if we run out of food/supplies?
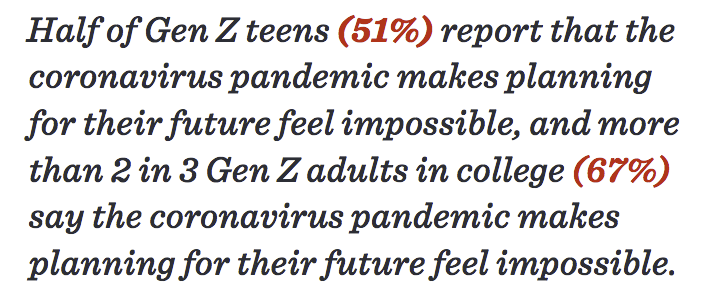
Even if your child isn't feeling anxiety about contracting COVID-19, they may be feeling just as out of control about other aspects of their life that have been impacted by COVID-19. According to the American Psychological Association's Stress on America report that surveyed the mental health impact of COVID-19, Generation Z teens (ages 13-17) are reporting severely disrupted plans impacting their future. Their "What if" questions may be: What if school doesn't reopen? What if I can't take the classes I need to take? What if I don't pass? What if I can't stay focused? What if I can't take the ACT/SAT? They also feel isolated and lonely, and may have fears about losing their friendships.
We strive for control when things feel out of control. We try to continue our lives, but keep getting met with barriers. When we find a solution for one barrier, we hit another wall and have to find a solution for that barrier. It’s mentally, physically, and emotionally exhausting. We’re grieving our losses while fearing what is to come next.
The need for certainty is a key trigger for anxiety.
We can’t be 100% certain in life. So we try to do things that give us the illusion of certainty to calm those “What if” questions (excessively checking social media, texting/seeking reassurance from friends, asking to watch the news, asking you repeatedly if there's enough food/supplies in the house, etc.). These behaviors may bring relief in the short-term, but then dissipate and the need to seek reassurance and certainty loops around again. The need for certainty triggers the fight or flight response, urging your child to fight to protect themselves. Only there seems to be no rest, and also no certainty.
Learning how to tolerate uncertainty is a key feature of anxiety treatments.
We are living in the midst of a pandemic, where there is ambient anxiety all around us. If you or your child is feeding the “What if” questions with behaviors meant to reassure them, then you are only feeding the anxiety, not the certainty. While COVID-19 is new to us, and research for an effective vaccine is pending, anxiety isn’t new, and treatments aren’t pending. We already know the evidence-based treatments that turn off the anxiety reinforcement loop. At ATSA, we use cognitive behavioral therapy and acceptance and commitment therapy to help you and your child tolerate anxiety and continue to live a valued life in the midst of the current pandemic.
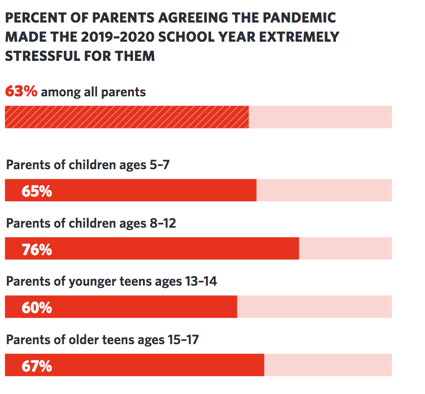
Impact of COVID-19 on Parents' Stress
Impact on Generation Z
The COVID-19 Anxiety Loop
Looking for the Adult Page? Click here
Questions? View FAQs View Insurance InformationClinical Procedures for COVID-19 Anxiety and Stress Evaluation and Outpatient Treatment
Free Phone Intake Consultation
Up to 30-min phone consultation so we can hear about your presenting issue, the symptoms you are experiencing, when they started, the severity of symptoms, and if we are the appropriate place for your treatment. The diagnostic intake process is discussed, and your insurance/billing questions are answered. If the treatment you need is within our scope of services, we begin the scheduling process. If it is deemed that we are not the appropriate place, we will provide you with referrals and resources to help you. We want to make sure to connect you with services, and that includes helping you find treatment elsewhere if that's what you need.
Free
CPT CODE: 0
Diagnostic Evaluation
A 90-min diagnostic intake interview with the child’s parents to assess symptoms, collect history, review systems (school, home, community), differential diagnosis, review of prior records, review parents’ families psychiatric histories, and follow up/clarify any questions that arose from reviewing the questionnaires parents/child/teen filled out before the intake session.
Starting at 295
CPT CODE: 90791
Child Observation and Intervention
Up to 60-min live behavioral observation(s) to assess and quantify the degree of anxiety, allowing us to define a baseline. Using a play-based model, additional questionnaires may be filled out for diagnostic purposes. Interventions are tested out, also using a play-based model, to assess the child's response to intervention for treatment planning purposes.
Starting at 195
CPT CODE: 90837
Parent Feedback Session, Guidance, and Treatment Planning
A 1-hour feedback session with parents is held which includes presenting diagnoses, symptom severity, diagnostic rule outs, and discussing the recommended treatment plan. Parents are asked for their specific goals for their child and what they hope to gain from treatment at ATSA. Decisions are made as to whether the child will start with therapy sessions only, allowing for the future addition of psychopharmacological treatment as an adjunct, or whether to start with combined treatment (or in rare cases to start with psychopharmacological treatment before CBT). Parents will be provided guidance on the behavioral techniques to implement at home and in the community with their child, to help maintain and generalize treatment gains. Parents are provided feedback about their child’s behavioral challenges and gains from the initial assessment sessions, and the specific techniques that will be used to successfully help their child overcome his/her specific barriers in the exposure process. Throughout treatment, parents are provided with additional feedback sessions to discuss next steps, including help with transfer of skills outside of the clinic setting.
Starting at 195
CPT CODE: 90846
Child Exposure Therapy Clinic Session
60 min exposure sessions to present the child with the phobic stimulus and begin the process of fear extinction. The key to exposure therapy is to activate new learning, which is done by presenting the child with the phobic stimulus, and assisting the child to approach (vs avoid) the stimulus. Parents are also taught how to facilitate approach coping and reduce enabling avoidance. Your therapist will use modeling, shaping, corrective feedback, and contingent reinforcement with child and parents. Our data show that when parents are involved in treatment, gains are more likely to transfer into the home and community settings.
Starting at 175
CPT CODE: 90837