Generalized Anxiety Disorder
Advanced Therapeutic Solutions for Anxiety provides therapy for the treatment of Generalized Anxiety Disorder.
Excessive anxiety and worry that is out of proportion to what would be expected is the hallmark of generalized anxiety disorder. Individuals with generalized anxiety disorder worry daily or almost daily. Their worries are about more than one situation, event, or activity (e.g., work/school performance worries, health, finances, being on time, being competent, the future, etc.) and can shift from one concern to another.
Children and adolescents with generalized anxiety disorder tend to worry excessively about their competence or quality of their performance, oftentimes interfering with school or sports. Their difficulty with focus may interfere with their ability to concentrate, and their performance suffers. Because they usually are eager to do well, not being able to focus on their work creates more worry, and a snowball effect can occur. If they’re not getting their work done, and feel overwhelmed, they may show avoidance of doing homework, going to school, etc. In sports, their worry may interfere with their focus, their mind can go blank, and they forget the sports play or dance routine. Because their performance (falling behind, missing a play, forgetting a dance) are perceived as not matching their values (doing well), they can feel restless and on edge. There may be excessive concerns about punctuality, perfectionism, seeking approval of their performance, being unsure of themselves, and doing and re-doing tasks because of their dissatisfaction with their performance. They may also have worries about catastrophic events (e.g., natural disasters) and show an excessive need for reassurance about all of the above.
The median age of onset for generalized anxiety disorder is 30 years. Prevalence for the disorder peaks in middle age, then declines in later years. The prevalence in adolescents is 0.9% (1 of 111) and in adults, it’s 2.9% (1 of 35). The onset of generalized anxiety disorder rarely occurs before adolescence. Because of its rarity in children, the diagnostic evaluation takes into account the other childhood anxiety disorders to determine if the worries they are experiencing aren’t better accounted for by another disorder (e.g., separation anxiety, social anxiety, obsessive-compulsive disorder).
Individuals with generalized anxiety disorder can have these associated symptoms:
- Restlessness, feeling keyed up, on edge
- Being easily fatigued
- Difficulty concentrating or mind going blank
- Irritability
- Muscle tension
- Sleep disturbance (difficulty falling or staying asleep, restless sleep, unsatisfying sleep)
Unlike generalized anxiety disorder, the worry that comes with everyday life does not include a great range of situations, does not last as long, is not excessive, can be put off when more pressing issues arise, and is not associated with the physical symptoms experienced by those with generalized anxiety disorder. The worries of a person with generalized anxiety disorder are more pervasive, pronounced, and physically distressing.
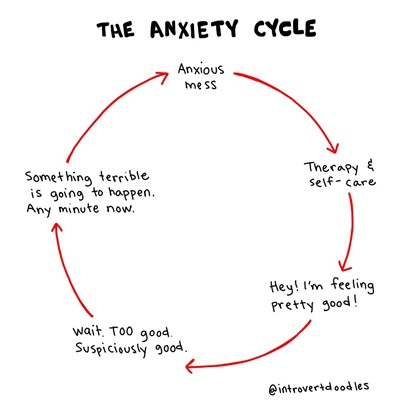
An individual with generalized anxiety has difficulty with focus and getting tasks done efficiently at home or work. The excessive worry takes over. Loved ones may hope to calm their family member by providing reassurance, but the reassurance feeds the anxiety. Because generalized anxiety disorder greatly impairs a person’s focus, concentration, and ability to work efficiently, a key component in treatment is mindfulness strategies that are used in therapy to help the individual learn to focus their awareness on the present moment. Behavioral interventions are also used to reduce the safety-seeking behaviors (e.g., reassurance) that interfere with learning. Therefore, acceptance-based behavioral therapy is the evidence-based treatment for generalized anxiety disorder.
Clinical Procedures for Generalized Anxiety Disorder Evaluation and Outpatient Treatment
Free Phone Intake Consultation
Up to 30-min phone consultation so we can hear about your presenting issue, the symptoms you are experiencing, when they started, the severity of symptoms, and if we are the appropriate place for your treatment. The diagnostic intake process is discussed, and your insurance/billing questions are answered. If the treatment you need is within our scope of services, we begin the scheduling process. If it is deemed that we are not the appropriate place, we will provide you with referrals and resources to help you. We want to make sure to connect you with services, and that includes helping you find treatment elsewhere if that's what you need.
Free
CPT CODE: 0
Diagnostic Evaluation
A 90-min diagnostic intake interview with the child’s parents to assess symptoms, collect history, review systems (school, home, community), differential diagnosis, review of prior records, review parents’ families psychiatric histories, and follow up/clarify any questions that arose from reviewing the questionnaires parents/child/teen filled out before the intake session.
Starting at 295
CPT CODE: 90791
Adolescent Intake Interview
A 60-min interview with the adolescent allows us to hear their perspective. Symptoms are assessed, and may include additional questionnaires for diagnostic clarification, allowing us to define a baseline. Interventions are tested out and discussed, using an age-appropriate model, to assess the adolescent's motivation and response to intervention for treatment planning purposes.
Starting at 195
CPT CODE: 90837
Parent Feedback Session, Guidance, and Treatment Planning
A 1-hour feedback session with parents is held which includes presenting diagnoses, symptom severity, diagnostic rule outs, and discussing the recommended treatment plan. Parents are asked for their specific goals for their teen and what they hope to gain from treatment at ATSA. Decisions are made as to whether the teen will start with therapy sessions only, allowing for the future addition of psychopharmacological treatment as an adjunct, or whether to start with combined treatment (or in rare cases to start with psychopharmacological treatment before CBT). Parents will be provided guidance on the behavioral techniques to implement at home and in the community with their child, to help maintain and generalize treatment gains. Parents are provided feedback about their child’s behavioral challenges and gains from the initial assessment sessions, and the specific techniques that will be used to successfully help their child overcome his/her specific barriers in the exposure process. Throughout treatment, parents are provided with additional feedback sessions to discuss next steps, including help with transfer of skills outside of the clinic setting.
Starting at 195
CPT CODE: 90846