Panic Disorder
Advanced Therapeutic Solutions for Anxiety provides therapy for the treatment of Panic Disorder.
Advanced Therapeutic Solutions for Anxiety provides therapy for the treatment of Panic Disorder.
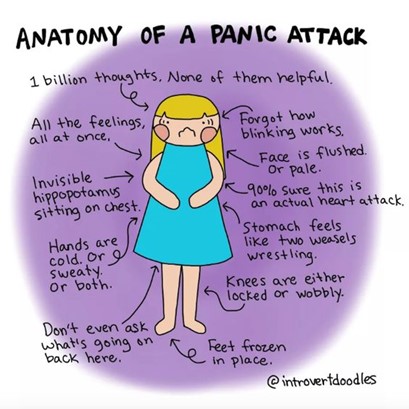
A panic attack is characterized as an abrupt surge of intense fear or intense discomfort, reaching a peak within minutes. During the surge, a person having a panic attack may experience heart palpitations, chest pains, sweating, trembling, shortness of breath, feelings of choking, and/or nausea or abdominal distress. They may feel dizzy, unsteady, light-headed, or faint. They could feel chills or heat sensations, numbness or tingling sensations (paresthesias), feelings of unreality (derealization) or being detached from oneself (depersonalization). During the surge, the person may fear that they are losing control, “going crazy” or fear that they’re dying.
A panic attack is scary. The sudden surge of such intense physical and cognitive symptoms that peak within minutes may leave a person to worry that it will occur again.
While panic attacks affect 11.2% of adults (1 of 11) in the U. S., not all adults go on to develop panic disorder. Panic disorder develops when a person has recurrent unexpected panic attacks and either worries persistently that the panic attack will occur again, or go to great lengths to ensure they don’t have one, such as avoiding physical exertion. They may also plan their schedule around making sure someone is available to help, just in case an unexpected attack happens. They may fear that they will indeed lose control, go crazy, embarrass themselves, or have a heart attack.
Panic disorder affects 2-3% (about 1 of 40) adults and adolescents, with the median age of 20-24 for when panic disorders may develop. Panic attacks are rare in children, and panic disorder is even rarer, with less than .4% (or about 1 of 260) occurring in children under age 14.
Panic disorder is treated with cognitive behavioral therapy, exposure therapy, and acceptance and commitment therapy. Psychoeducation about anxiety helps to increase the person’s understanding of what a panic attack is and how the cycle runs. Learning about the thoughts-emotions connection, particularly how the fear thoughts (e.g., “I’m having a heart attack”) feed the fear, which then triggers more physical symptoms, helps the person understand how both work to feed off each other during a panic attack. During exposure therapy, the feared event (i.e., panic attack) is simulated by bringing on physical sensations such as spinning around in circles to feel dizzy or running in place to have shortness of breath, and then applying the cognitive reappraisals and progressive muscle relaxation to calm the sensations. Gaining this understanding helps a person feel more in control during a panic attack, and helps them learn how to turn off the attack before it peaks.
Clinical Procedures for Panic Disorder Evaluation and Outpatient Treatment
Free Phone Intake Consultation
Up to 30-min phone consultation so we can hear about your presenting issue, the symptoms you are experiencing, when they started, the severity of symptoms, and if we are the appropriate place for your treatment. The diagnostic intake process is discussed, and your insurance/billing questions are answered. If the treatment you need is within our scope of services, we begin the scheduling process. If it is deemed that we are not the appropriate place, we will provide you with referrals and resources to help you. We want to make sure to connect you with services, and that includes helping you find treatment elsewhere if that's what you need.
Free
CPT CODE: 0
Diagnostic Evaluation
A 90-min diagnostic intake interview with the child’s parents to assess symptoms, collect history, review systems (school, home, community), differential diagnosis, review of prior records, review parents’ families psychiatric histories, and follow up/clarify any questions that arose from reviewing the questionnaires parents/child/teen filled out before the intake session.
Starting at 295
CPT CODE: 90791
Adolescent Intake Interview
A 60-min interview with the adolescent allows us to hear their perspective. Symptoms are assessed, and may include additional questionnaires for diagnostic clarification, allowing us to define a baseline. Interventions are tested out and discussed, using an age-appropriate model, to assess the adolescent's motivation and response to intervention for treatment planning purposes.
Starting at 195
CPT CODE: 90837
Parent Feedback Session, Guidance, and Treatment Planning
A 1-hour feedback session with parents is held which includes presenting diagnoses, symptom severity, diagnostic rule outs, and discussing the recommended treatment plan. Parents are asked for their specific goals for their teen and what they hope to gain from treatment at ATSA. Decisions are made as to whether the teen will start with therapy sessions only, allowing for the future addition of psychopharmacological treatment as an adjunct, or whether to start with combined treatment (or in rare cases to start with psychopharmacological treatment before CBT). Parents will be provided guidance on the behavioral techniques to implement at home and in the community with their child, to help maintain and generalize treatment gains. Parents are provided feedback about their child’s behavioral challenges and gains from the initial assessment sessions, and the specific techniques that will be used to successfully help their child overcome his/her specific barriers in the exposure process. Throughout treatment, parents are provided with additional feedback sessions to discuss next steps, including help with transfer of skills outside of the clinic setting.
Starting at 195
CPT CODE: 90846
Adolescent Exposure Therapy Clinic Session
60 min exposure sessions to present the adolescent with the phobic stimulus and begin the process of fear extinction. The key to exposure therapy is to activate new learning, which is done by presenting the adolescent with the phobic stimulus, and assisting the adolescent to approach (vs avoid) the stimulus, using a hierarchical approach. Motivational interviewing may be applied to foster rapport and trust in preparation for exposures, particularly when exposures become more challenging as we move up the hierarchy. Parents are also taught how to facilitate approach coping and reduce enabling avoidance. We will use modeling, shaping, corrective feedback, and contingent reinforcement with adolescent and parents. Our data show that when parents are involved in treatment, gains are more likely to transfer into the home and community settings.
Starting at 175
CPT CODE: 90837
Adolescent Exposure Therapy in Home, School, or Community Settings
60-min exposure sessions provided in the school, home, or community setting to help transfer treatment gains into these domains. To increase transfer of treatment gains, reduce avoidance of the phobia across settings, and reduce others rescuing the adolescent from approaching the phobia (to rescue them from distress), in-vivo and in-situ exposure therapy is most effective. Not only does the adolescent develop distress tolerance, new learning, and fear extinction, so do the adults in these settings, which helps them reduce rescuing and enabling. We will train school staff on how to appropriately prompt, monitor, and reinforce your adolescent's approach behavior with guidance via modeling and demonstrating use of skills. Home visits are used to help adolescents and parents use skills at home, and Community sessions provide exposure practice in new settings.
Starting at 185 + travel
CPT CODE: 90837