Selective Mutism
Advanced Therapeutic Solutions for Anxiety are specialists in providing PCIT-SM therapy for the treatment of Selective Mutism.
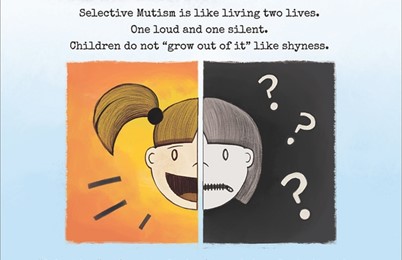
Selective Mutism is the fear of speaking in specific social situations, despite the ability to speak, and affects 1 of 140 children. Children with selective mutism are chatterboxes and may "take center stage" at home, but when out in public, in school, or when others come to their house, they become uncharacteristically mute. These are kids who like to lead and they possess incredible determination - but when in school, they become reticent, mute, and a follower instead of a leader (that is, if they are not avoiding their peers altogether).
Selective Mutism (SM) was first recognized by the American Psychological Association in the Diagnostic Statistical Manual of Mental Disorders in 1980 as Elective Mutism, and later in 1994 as Selective Mutism. Before 1980, SM cases were either misdiagnosed or not diagnosed at all. Since then, knowledge and understanding of SM has grown. Experts now recognize selective mutism as an anxiety disorder, and 2013 it was moved from the now retired Early Childhood Disorders to the Anxiety Disorders category in the 5th edition of the DSM. It is not uncommon for a child to be diagnosed with both Selective Mutism and Social Phobia, as the correlation exceeds 90%.
As SM knowledge grows, so do effective treatments. Understood as a phobia, effective SM treatments take into account the power of exposure-based therapy, which includes taking systematic steps towards facing one's fear. Systematically planned steps gradually increase exposure and lead to new learning, reducing the fear response.
Here are some questions to ask yourself about your child:
- Does your child speak at home but become excessively quiet when others are around, and doesn't seem to warm up?
- Does your child fail to speak to peers in school or community settings?
- Does your child cling to you/tug you excessively in public settings?
- Does your child look around before talking to you, or make sure others aren't close by to hear?
- Does your child appear frozen, stuck, or unsure when in a social or public activity?
- Does your child's teacher say he/she is grunting or making noises to communicate, but not talking?
- Does your child's teacher say he/she uses nonverbal body language to communicate (pointing, gesturing, head nods/shakes) but does not talk, even after the first month of school?
Answering "yes" to any of these questions may indicate a possibility of selective mutism. Selective mutism is usually first recognized when the child starts preschool. Teachers typically report that the child is not talking but using nonverbal means to communicate instead. Parents usually report that their child talks fine at home. Parent education and early intervention is pivotal in the trajectory of this disorder. Selective mutism can be successfully treated, but don't wait - early intervention yields best results. There is no evidence that children grow out of selective mutism. They may improve some with age, but remain clinical. Click here to read about selective mutism in adults.
Make sure you select a provider who knows how to treat selective mutism.
All ATSA clinicians are certified trainers and therapists in providing PCIT-SM for the treatment of selective mutism. ATSA is also the first in the nation to replicate Steven Kurtz Ph.D.’s Brave Buddies program, called Adventure Camp, bringing this 5-day in-vivo, in-situ school simulation group exposure therapy program to Chicago in 2011. Patients who receive selective mutism treatment at ATSA average about one year of services when following the clinician’s treatment recommendations, (the frequency of services depends on the needs of the patient and child/parent responsivity to treatment) before they can ‘graduate’ from specialty services
Clinical Procedures for Selective Mutism Evaluation and Outpatient Treatment
Diagnostic Evaluation
A 90-min diagnostic intake interview with the child’s parents to collect history, review of systems, differential diagnosis, review of prior records, review of sample videotape of child functioning, parents’ families psychiatric histories, especially in regards to SM and social anxiety.
Starting at 295
CPT CODE: 90791
Child Observation & Parent Training
Up to 60-min live behavioral observation(s) to assess and quantify the degree of mutism with and without the presence of a trained confederate “stranger,” (i.e., the therapist) allowing us to define baseline response rate to different question types, rate, latency and volume of speech with and without stranger present. Live training and modeling of basic exposure skills is provided to parents during this session. In this session and subsequent therapy sessions, Parents are taught, practice, and demonstrate the basics of the requisite prompting, monitoring, and reinforcement skills used by staff. Staff use modeling, shaping, corrective feedback, and contingent reinforcement with parents to train them in these skills.
Starting at 195
CPT CODE: 90837
Parent Feedback Session, Guidance, and Treatment Planning
A 1-hour feedback session with parents is held which includes presenting diagnoses, symptom severity, diagnostic rule outs, and discussing the recommended treatment plan. Parents are asked for their specific goals for their child and what they hope to gain from treatment at ATSA. Decisions are made as to whether the child will start with therapy sessions only, allowing for the future addition of psychopharmacological treatment as an adjunct, or whether to start with combined treatment (or in rare cases to start with psychopharmacological treatment before CBT). Parents will be provided guidance on the behavioral techniques to implement at home and in the community with their child, to help maintain and generalize treatment gains. Parents are provided feedback about their child’s behavioral challenges and gains from the initial assessment sessions, and the specific techniques that will be used to successfully help their child overcome his/her specific barriers in the exposure process. Throughout treatment, parents are provided with additional feedback sessions to discuss next steps, including help with transfer of skills outside of the clinic setting.
Starting at 195
CPT CODE: 90846
SM Therapy Session
60 min exposure sessions to condition the child to speak to parent in the presence of the therapist, then systematically over several sessions fading the parent out so the child is talking to the therapist in the absence of the parent. During these sessions, parents build on the basics taught during the Parent Training session, practicing and demonstrating to mastery the requisite prompting, monitoring, and reinforcement skills used by staff. Staff continue to use modeling, shaping, corrective feedback, and contingent reinforcement with child and parents. Our data show that we are able to establish verbal behavior within 6 sessions with the majority of our patients.
Starting at 175
CPT CODE: 90837
SM Therapy School Visit / Community Visit
60-min exposure sessions provided in the school, home, or community setting to help transfer treatment gains into these domains. By nature of the disorder, SM symptoms occur selectively across environments. To increase transfer of treatment gains and help establish and maintain verbal behavior in other settings, in-vivo and in-situ exposure therapy is most effective. Similar to the clinic visit, your ATS Therapist works with school staff to train them how to appropriately prompt, monitor, and reinforce your child’s verbal behavior with guidance via modeling and demonstrating use of skills. Community visits are used to help parents use skills in public, and/or provide exposure practice in new settings. These sessions are important to condition the child to speak in more than one setting, fostering generalization of verbal behavior in multiple settings. Our data show that patients who receive clinic, school, and community sessions show increased self-confidence, less inhibition, and overall significant improvement in verbal behavior and social interaction.
Starting at 175 + travel
CPT CODE: 90837