Selective Mutisim
Advanced Therapeutic Solutions for Anxiety are specialists in providing exposure therapy for the treatment of Selective Mutism.
Selective mutism is the fear of speaking in specific social situations, despite the ability to speak. Selective mutism used to be categorized under the “Disorders in Early Childhood” in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). When DSM-IV was revised to DSM-5, which involved research and collaboration from experts in the field of psychology, the early childhood disorders classification was retired, and selective mutism was moved. It is now housed under the anxiety disorders classification.
We know from current research that there is no evidence to support “spontaneous” recovery; in other words, there is no evidence to support the notion that a child will grow out of selective mutism. That is why we do see selective mutism impacting older ages; at ATSA we have treated teens and adults with selective mutism.
We also know from research and from clinical practice that the anxious-avoidance loop of not talking becomes more entrenched as time goes on. “If you don’t use it, you lose it” is how one young adult explained their experience growing up with selective mutism, eventually realizing that “losing it” didn’t just apply to talking, but also applied to driving, going out on their own, moving away to college, and “experiencing life.” As with many older individuals with selective mutism, the young adult realized that the older they got, the smaller their world was becoming.
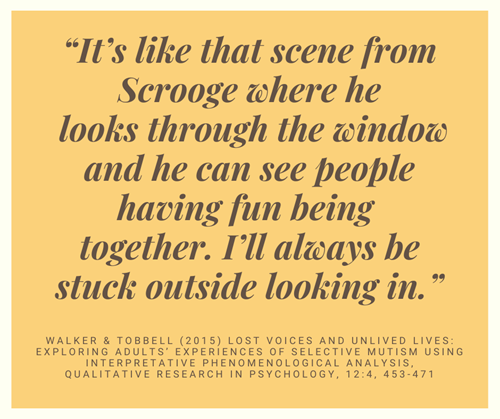
The research article, “Lost Voices and Unlived Lives: Exploring Adults’ Experiences of Selective Mutism using Interpretative Phenomenological Analysis” by Walker & Tobbell (2015) offers a view of how adults are impacted by selective mutism. It is an emotional read, especially if you love someone with selective mutism, but it is an important reminder that not pursuing appropriate, evidence-based treatment can be risky. The wait-and-see approach is not the solution, nor is going to a provider who is not familiar with how to treat selective mutism.
At ATSA, we know what to do. A parent once said, “When I ask other providers questions, they always say they don’t know or can’t know yet, and we just have to wait and see. When I ask you the same questions, I love that I get an answer, that you know what you’re talking about, and that there are things we can still do. You always give us an answer, and then we feel hopeful again.”
Treatment for selective mutism in older ages is a very specialized area. Ideally, treatment involves the participation of the individual with selective mutism and their relative who talks for them, since both are in an anxious-avoidance loop. Selective mutism is treated with exposure therapy in which the individual is guided through a hierarchical ladder of verbalizing first with their relative, then transferring the verbal behavior to the therapist, and continuing on with generalizing speaking across people, places, and activities. Medication is often recommended to bring the anxiety down enough so that the individual can be more accessible to the behavioral therapy, including exposure therapy, cognitive-behavioral therapy, and acceptance and commitment therapy.
Clinical Procedures for Selective Mutisim Evaluation and Outpatient Treatment
Free Phone Intake Consultation
Up to 30-min phone consultation so we can hear about your presenting issue, the symptoms you are experiencing, when they started, the severity of symptoms, and if we are the appropriate place for your treatment. The diagnostic intake process is discussed, and your insurance/billing questions are answered. If the treatment you need is within our scope of services, we begin the scheduling process. If it is deemed that we are not the appropriate place, we will provide you with referrals and resources to help you. We want to make sure to connect you with services, and that includes helping you find treatment elsewhere if that's what you need.
Free
CPT CODE: 0
Diagnostic Evaluation
A 90-min diagnostic interview is conducted to assess the presenting problem, symptoms severity (onset, duration, frequency), review areas of life that have been impacted (daily functioning, work, home), collect history, including family history of anxiety or depression, and review what you hope to gain from treatment at ATSA. Specific questions and or measures may be administered during the session for diagnostic purposes.
Starting at 295
CPT CODE: 90791
Treatment Planning Session
A 60-min session to review how the first sessions have felt to you, present hypotheses, and collaborate on a treatment plan. Treatment approaches may include Acceptance and Commitment Therapy (ACT), Cognitive Behavioral Therapy (CBT), Exposure and Response Prevention (ERP). Treatment dose is also discussed, specifically if weekly 60-min outpatient sessions will be effective, or if intensive doses (e.g., 3-hr sessions) should be considered. Likewise, location of where sessions should occur for most effective outcome is also discussed and planned out. Decisions are made as to whether to start with therapy sessions only, allowing for the future addition of psychopharmacological treatment as an adjunct, or whether to start with combined treatment, (or in rare cases to start with psychopharmacological treatment before CBT, ACT, or ERP).
Starting at 175
CPT CODE: 90837
Exposure Clinic Session
60 min exposure sessions to present you with the phobic stimulus and begin the process of fear extinction. The key to exposure therapy is to activate new learning, which is done by presenting the phobic stimulus, and assisting you to approach (vs avoid) the stimulus, using a hierarchical approach. With repeated exposures, you gain distress tolerance and fear extinction. Additional therapies (e.g., ACT, CBT) may be applied to keep you focused and motivated in preparation for exposures, particularly when exposures become more challenging as we move up the hierarchy. When possible, family members will be included to learn how to facilitate approach coping and reduce enabling avoidance. Our data show that when family members learn how to support you, you are more likely to maintain your treatment gains.
Starting at 175
CPT CODE: 90837
Exposure Therapy in Home or Community Settings
60-min exposure sessions provided in the home or community setting to help transfer treatment gains into these domains. To increase transfer of treatment gains, reduce avoidance of the phobia across settings, and reduce others rescuing you from approaching your phobia (to rescue you from distress), in-vivo and in-situ exposure therapy is most effective. Not only will you develop distress tolerance, new learning, and fear extinction, so will others in these settings, which helps them reduce rescuing and enabling. Home visits are used to help you use skills at home, and Community sessions provide exposure practice in new settings.
Starting at 185 + travel
CPT CODE: 90837